Chronic prostatitis is one of the most common diseases among mature men. Inflammation of the prostate significantly reduces the quality of life, becoming a cause of psychosomatic and sexual disorders. The lack of sufficient information about the nature of this disease makes the treatment of chronic prostatitis a difficult task that requires a lot of patience from both the patient and his doctor.
Prostatitis is an inflammatory-degenerative lesion of the prostate.
Classification
The National Institutes of Health (NIH USA) has developed and proposed the following classification of chronic prostatitis:
- chronic bacterial prostatitis;
- chronic nonbacterial prostatitis (with and without signs of inflammation);
- chronic asymptomatic prostatitis.
Modern andrologists adhere to this classification in the diagnosis and treatment of inflammatory diseases of the prostate. Acute prostatitis stands out. Knowing which category the identified pathology belongs to, the doctor will be able to choose the optimal treatment regimen and achieve significant success in the treatment of the disease.
Causes and risk factors
The division into bacterial and nonbacterial chronic prostatitis is not accidental. Various causes of the disease determine the tactics of treatment and greatly affect the outcome of the disease.
Chronic bacterial prostatitis
Chronic bacterial prostatitis occurs in 10-15% of patients. The immediate cause of the development of the disease is the penetration of pathogenic and opportunistic flora into the prostate. By definition, the prostate does not contain bacteria. Prostate infection is possible through the urethra, as well as hematogenous and lymphogenic. The following microorganisms are most often detected during the examination:
- Escherichia coli (up to 95%);
- Proteus;
- klebsiella;
- pseudomonas.
Representatives of gram-positive flora (staphylococci, streptococci) are quite rare. In some cases, the growth of two or more microorganisms (mixed infection) is recorded. Possible infection with pathogenic flora (chlamydia, trichomonas, gonococcus and others).
Most of the microorganisms detected during the examination are representatives of the normal microflora. Under normal conditions they do not harm the body and exist peacefully on the mucous membranes of the urinary system and digestive tract. Under certain conditions, the conditionally pathogenic flora grows and multiplies, which leads to inflammation of the prostate tissue and the appearance of all the symptoms of the disease.
Risk factors for the development of chronic bacterial prostatitis:
- disrespect for personal hygiene;
- hypothermia;
- genital trauma;
- inflammatory diseases of the urinary system;
- the presence of STIs.
All this leads to a decrease in local and general immunity and the natural reproduction of opportunistic flora in the prostate. It is not excluded that the infection can enter through the urethra in inflammatory diseases of the genital tract. The probability of developing prostatitis increases with existing urethritis, cystitis, coliculitis.
Chronic nonbacterial prostatitis
There are several theories about the origin of this form of the disease:
- Theory of chemical inflammation. . . The discharge of urine into the prostate during urination leads to the deposition of urine and the development of inflammation. Urethro-prostatic reflux is facilitated by narrowing of the urethra (stricture) and other developmental abnormalities.
- Immunity theory. . . The version is based on autoimmune damage to prostate tissue as a result of exposure to bacterial antigens. Hereditary predisposition to this form of pathology is considered.
- Neurogenic theory. . . Violation of innervation in the pelvic area causes blood stagnation in the organs and leads to the development of prostatitis.
In the development of nonbacterial prostatitis, the following risk factors also deserve special attention:
- long sedentary work;
- inactive lifestyle;
- bad habits;
- stress and emotional overload;
- prolonged sexual abstinence.
These risk factors cause the development of congestion in the prostate, leading to a violation of the microcirculation in the pelvic organs. Microbial factor plays a role only in the initial stages of disease development. In the future, its importance decreases, and autoimmune processes and trophic disorders in prostate tissues come to the fore.
According to statistics, 85-90% of men have non-bacterial chronic prostatitis (which is not directly related to infection with pathogenic or opportunistic bacteria).
Symptoms
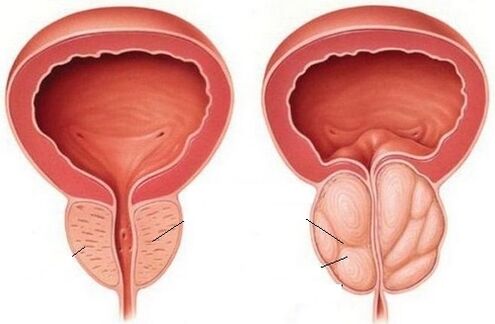
Chronic prostatitis occurs mainly in men aged 25-40 years. With age, the probability of developing the disease increases. In old age, inflammation of the prostate is often combined with an adenoma - a benign tumor of the prostate.
Signs of chronic prostatitis:
- dull aching pains in the lower abdomen;
- irradiation of pain in the groin, scrotum, perineum, lower back, sacrum;
- increased discomfort during intercourse and during stool.
Urinary disorders are very characteristic:
- frequent urination;
- excretion of urine in small meals;
- feeling of incomplete emptying of the bladder;
- the appearance or intensification of pain when urinating;
- sluggish and intermittent stream of urine.
The latter symptom is characteristic of prostate adenoma, which often occurs in the background of chronic prostatitis.
With a long course of the disease, there is a disorder in the sexual sphere:
- decreased libido;
- worsening of erection;
- reducing the duration of the relationship;
- premature ejaculation;
- withdrawal pain in the lower abdomen after ejaculation;
- lack of spontaneous morning erection.
Chronic prostatitis is one of the leading causes of erectile dysfunction, in which a man cannot achieve and maintain an erection sufficient for complete sexual intercourse. Such a condition significantly disrupts the course of life, can cause depression and other psycho-emotional disorders.
Chronic asymptomatic prostatitis occurs without any clinical manifestations. The disease is discovered accidentally during an examination by a urologist. Despite the absence of symptoms, inflammation of the prostate can lead to serious complications, erectile dysfunction and other health problems.
Complications
Initiated prostatitis provokes the development of such conditions:
- prostate abscess;
- cystitis and pyelonephritis (inflammation of the bladder and kidneys);
- vesiculitis (inflammation of the seminal vesicles);
- erectile dysfunction;
- infertility.
The earlier the disease is detected and treatment is started, the better the chances of a favorable outcome of the disease.
Diagnosis
The following methods are used to detect chronic prostatitis:
Examination by a urologist
In a face-to-face meeting, the doctor focuses on the patient’s complaints. The external genitalia are examined and a digital rectal examination of the prostate is performed. On palpation, the doctor assesses the size and shape of the gland. In the case of chronic prostatitis, the organ will be slightly enlarged. The procedure is combined with the collection of prostate secretions for microbiological examination.
A sample of four glasses
The main method that allows you to recognize the inflammatory process in the prostate and distinguish it from other diseases. The collection of materials takes place in several stages. In the morning, after 5-6 hours of abstinence from going to the toilet, the man urinates in two jars - for the first (initial) and for the second (middle) portion of urine. In the first part, the contents of the urethra are flushed, in the second - the bladder. A third of the urine is collected after a prostate massage and allows you to assess the condition of the prostate. The prostate secretion is collected separately for bacteriological culture.
In the analysis of urine, two parameters are assessed: the number of leukocytes and erythrocytes. In prostate disease, the number of white blood cells increases in the third part of the urine. Their number in the field of view usually does not exceed 10.
Microbiological examination
When performing the test of three glasses, not only the number of leukocytes is estimated, but also the material for bacteriological inoculation is taken. If you suspect chronic prostatitis, your doctor is particularly interested in a third of your urine. Based on the results of the examination, the doctor can identify the cause of the disease and select the optimal antibiotic therapy.
The diagnostic value is the identification of opportunistic bacteria in a titer greater than 10.3CFU / ml or detection of unambiguously pathogenic microorganisms in any quantity.
Bacteriological culture of prostate secretion

Bacteriological seeding of prostate fluid enables assessment of the nature of the process (infectious or not) and determination of the type of pathogen.
Before taking a third of the urine during a prostate massage, the doctor takes the secreted secretion for a bacteriological examination. The obtained result also allows to establish the diagnosis and treatment tactics.
Diagnostic criteria for chronic bacterial prostatitis:
- Detection of opportunistic microorganisms in the third part of urine or prostate secretion in a titer above 103CFU / ml.
- Detection of opportunistic bacteria in the third part of urine or prostate secretion, the number of which is significantly (10 times) higher than in the second part of urine.
- Identification of pathogenic microorganisms in the third part of urine or prostate secretion.
Ultrasound
Ultrasound examination allows you to assess the size of the organ and identify the accompanying pathology. Chronic prostatitis is often combined with prostate adenoma - a benign tumor.
Principles of treatment
The goal of chronic prostatitis therapy is to eliminate the inflammatory process, activate blood flow and improve organ nutrition. When pathogens or opportunistic microorganisms are detected in high titers, they are eliminated. Special attention is paid to the correction of lifestyle and stimulation of the body's defenses.
Drug treatment
The following medications are used to treat chronic prostatitis:
- Antibacterial drugs are selected taking into account the identified pathogen.
- Anti-inflammatory drugs to reduce inflammation and relieve pain.
- Means that facilitate urination (alpha-blockers, which relax the urethral muscles and stimulate the outflow of urine).
- Agents that increase blood flow in the pelvic organs.
The choice of antibiotic will depend on the pathogen identified. When choosing a drug, its ability to penetrate the hematoprostatic barrier and accumulate in prostate tissues should be taken into account. These conditions are met by agents from the fluoroquinolone group. Macrolides and tetracyclines are also used to treat chronic prostatitis.
According to the recommendations of the European Association of Urology, the course of antibacterial therapy should be at least 2 weeks after the establishment of a preliminary diagnosis.
Upon receipt of the results of bacteriological examination and confirmation of the bacterial nature of the disease, treatment lasts up to 4-6 weeks. This approach enables not only the removal of the cause of the disease, but also the prevention of the recurrence of prostatitis.
Unfortunately, antibiotic therapy is not always effective. Many microorganisms have long been successfully present in the secretion of the prostate and acquire resistance to antibiotics. Bacteria form special biofilms and form colonies of microorganisms covered with a complex polysaccharide structure. Most antibacterial drugs are unable to penetrate this biological barrier, which significantly reduces the effectiveness of therapy. This problem can be avoided by applying modern antibiotics, which can not only penetrate the prostate tissue and heat up in it, but also pass through biofilms and infect bacteria that are under such serious protection.
Drug-free therapy
Among non-drug medications, special attention is paid to prostate massage. The procedure stimulates the supply of the prostate gland, removes congestion and facilitates the secretion. The combination of massage and long-term use of antibacterial drugs is the main way to relieve a man from the unpleasant symptoms of chronic prostatitis.
Physiotherapeutic methods of influence are used in the treatment of chronic prostatitis together with healing effects. A good effect is seen from the use of ultrasound, laser beam, radio waves and electromyostimulation. Impact prostate massage (UHM) is very popular. Physiotherapy is especially indicated in the case of erectile dysfunction as one of the complications of prostatitis.
Special attention is paid to diet in the treatment of prostatitis. The following foods should be excluded from the diet:
- alcohol;
- spicy, spicy foods;
- fried and fatty foods (including fatty meats and fish).
Salt consumption is limited to 5 g per day. Priority is given to fresh vegetables and fruits, herbs. Mating is recommended.
The diet will speed up recovery, strengthen immunity and help the body cope with the stress caused by antibiotics during the treatment of the disease.
ethnoscience
Not all men go to the doctor when symptoms of prostatitis appear. Often men prefer to treat themselves with folk methods, using the knowledge base from numerous forums, relying on the advice of friends, relatives and neighbors. Neglecting one's own health, rejecting rational antibiotic therapy, and other traditional methods of exposure threatens to develop complications and worsen the general condition. Prostatitis that is not cured in time can cause erectile dysfunction. Is it worth the risk if you can visit a doctor on time and solve the problem with minimal losses?
Of course, among the methods of traditional medicine there are some aspects that deserve special attention. Modern urology recognizes the effectiveness of many herbs in treating chronic prostatitis. Experts recommend herbal preparations based on the following ingredients:
- pumpkin oil;
- evergreen round-leaved;
- garden parsley;
- St. John's wort perforatum;
- Canadian gold rod;
- licorice root;
- echinacea.
Individually or in combination, these components stimulate blood flow in the pelvic organs, remove congestion and stimulate the immune system.
Phytopreparations will not rid the body of pathogenic bacteria, but they will help eliminate the symptoms of the disease.
In combination with antibacterial drugs and prostate massage, herbal medicines significantly improve the general condition and speed up recovery.
Prevention
The following recommendations will help reduce the risk of developing chronic prostatitis:
- Hypothermia of the whole body and genital area, pelvis and lower extremities must not be allowed. In the cold season it is worth wearing thermal underwear.
- It is necessary to follow the rules of intimate hygiene and use condoms to protect against STIs. The best prevention of infection will be to reject casual sex.
- You should take care of your health and treat all diseases of the genital area in time.
- It will not be superfluous to follow a diet (give up spicy, fried and fatty foods), as well as keep the body in good shape (playing sports, fitness, walking).
All men over the age of 30 are recommended to see a urologist regularly (at least once a year). If you experience any unpleasant symptoms, you should see your doctor as soon as possible.
FAQ
Can chronic prostatitis be cured?
Contrary to popular belief, chronic prostatitis can be successfully treated. If you follow all the doctor's recommendations, you can get rid of the unpleasant symptoms of prostatitis and significantly improve your quality of life.
Can chronic prostatitis be asymptomatic?
Yes, this variant of the disease is detected only after examination by a urologist.
Is chronic prostatitis in a partner dangerous for a woman?
Sexually transmitted infections are often the cause of chronic prostatitis. If a pathogenic agent is identified, both partners must undergo treatment. Otherwise, there is a risk of infection, and the effectiveness of the therapy is reduced due to the recurrence of the disease.
Is sexual intercourse with chronic prostatitis possible?
Yes, if the general condition allows and there are no problems in the sexual sphere (erectile dysfunction).
Is it possible to conceive a child with chronic prostatitis?
Yes, if the prostate function is preserved and its secret is fully developed. An examination and treatment by a urologist is recommended before conceiving a child. The infection that caused the development of prostatitis is easily transmitted to a woman. Intrauterine infection of the fetus can cause developmental abnormalities and termination of pregnancy.
How does chronic prostatitis affect potency?
Chronic inflammation of the prostate threatens the development of erectile dysfunction. With such pathology there is a decrease in libido, the frequency and strength of erections decreases, orgasms become painful. In advanced cases, sexual activity becomes impossible.
Can chronic prostatitis be cured without antibiotics?
Antibiotic therapy is considered one of the key ways to treat chronic prostatitis. In most cases, it is impossible to deal with the disease without antibiotics.
Can chronic prostatitis be cured with folk remedies?
Solving chronic prostatitis with traditional medicine alone will not succeed. In order to achieve the optimal effect, complex treatment with antibiotics, herbal preparations, anti-inflammatory drugs and physiotherapeutic methods is carried out.



























